Research Highlights
Einstein Researchers Attack Cancer-Causing Proteins
Class I phosphoinositide 3-kinases (class I PI3Ks) may be the most important molecules you’ve never heard of. These cellular proteins serve mainly as signaling nodes, meaning they sense when certain receptors on the cell membrane receive signals and then relay those signals into the cell.
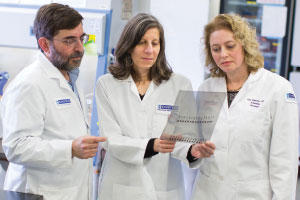
From left: Drs. Jonathan Backer, Anne Bresnick and Kira Gritsman are studying PI 3-kinases, a family of enzymes that play essential roles in the life of a cell. Abnormal PI 3-kinases can start a chain reaction that leads to cancer.The class I PI3Ks accomplish that latter step by adding a phosphate group (an amalgam of phosphorus and oxygen atoms) to specific lipid molecules in cell membranes—which sounds simple. But this modest action, known as phosphorylation, has profound consequences for a cell’s health, since it can activate pathways involved in growth, proliferation, motility, survival and the transport of substances within the cell. Not surprisingly, glitches in PI3K pathways can cause things to go very wrong. Indeed, class I PI3Ks have been linked to the genesis and spread of various cancers.
Given the importance of class I PI3Ks, several researchers at the Albert Einstein Cancer Center are studying these proteins and the genes that encode them. Two of those researchers —Drs. Jonathan Backer and Anne Bresnick—recently received a four-year, $1.2 million National Institutes of Health grant to investigate the mechanisms that govern the activity of p110-beta, one of the four class I PI3K members.
Blocking a Cancer-Causing Signal
In normal cells, a gene called PTEN keeps class I PI3Ks in check. But it’s not uncommon for PTEN to undergo damaging mutations that take the brakes off PI 3-kinase signaling and send cell growth into overdrive—which, of course, is one of the hallmarks of cancer. p110β excites cancer researchers because it specifically activates cell growth in a subset of tumors—those that contain PTEN mutations.
“The question we want to answer is, exactly how does p110β drive cell growth in tumors with PTEN mutations?” said Dr. Bresnick, professor of biochemistry and director of the Belfer Institute for Advanced Biomedical Studies. “Most researchers have focused on p110β’s kinase activity and have looked for compounds that can inhibit this process. The idea is that if you can block this function of p110β, you can slow or stop cancer progression.” This approach is currently being explored in clinical trials testing the effectiveness of kinase inhibitors. However, tumors develop resistance due to mutations in the target kinases that make them insensitive to the inhibitors.
Disrupting a Cancer-Causing Protein Complex

This article originally appeared in the winter/spring 2016 Albert Einstein Cancer Center newsletter.Drs. Bresnick and Backer are investigating a different approach to inhibiting p110β signaling. In cells, p110β activity is regulated by its binding to another signaling molecule, a two-protein complex called G-beta-gamma. A few years ago, Dr. Backer identified the site on p110β to which Gβγ binds. He then created a mutation in the gene for p110β that prevents it from hooking up with Gβγ—a genetic engineering feat that provides a novel way to examine the combined roles of p110β and Gβγ in cancer.
“It turns out that disrupting binding between p110β and Gβγ works to prevent normal cells from becoming cancerous, at least in tissue culture,” said Dr. Backer, chair and professor of molecular pharmacology and professor of biochemistry.
Drs. Backer and Bresnick are now studying whether this will hold true in mouse models of prostate and endometrial cancers driven by PTEN mutations. If so, the next step will be to identify compounds that inhibit the coupling of p110β and Gβγ. “That’s the hard part, since the region of p110β that binds to Gβγ cannot be seen in crystal structures of p110β, making it difficult to design a drug,” said Dr. Bresnick.
Precision Medicine
Any drug that might emerge from this study would probably be effective against a very specific set of cancers. While this may sound like a drawback, it’s exactly the point of precision medicine, which departs from the traditional “one-size-fits-all” approach to therapy.
“Until recently, most cancer therapy has been aimed at a general property of all tumors—they grow fast,” said Dr. Backer. “Unfortunately, treatments that disrupt cell division have lots of side effects, because they also impact other parts of our body that have high rates of cell turnover, like the gut and bone marrow. It’s becoming increasingly clear that knowing the mutational status of a patient’s tumor will be critical to deciding what drugs to use. Studies that explain how different members of the PI3K family contribute to tumor formation and metastasis are a step in that direction.”
PI3Ks and Leukemia
Class I PI3Ks may also hold the key to new treatments for acute myeloid leukemia (AML), the most common bone marrow cancer in adults. AML has a five-year survival rate of only 25 percent. Making matters worse, current therapies are extremely toxic and debilitating, and some patients die due to treatment-related complications.
While many different genetic abnormalities can lead to AML, up to 80 percent of AML cases have a common feature: activation of the PI3K pathway. This would seem to suggest that inhibiting PI3K signaling could help treat AML. Yet studies show that this treatment approach may harm normal bone marrow stem cells as well as the “bad” stem cells that form leukemic blood cells—an unacceptable trade-off, since stem cells are needed to create new normal blood cells.
So how does one target this pathway only in diseased cells? Dr. Kira Gritsman, assistant professor of medicine (oncology) and of cell biology, who joined Einstein in 2014, is working on an answer.
Targeting Precise Proteins
“It’s now known that all four of the class I PI3K family members are found in blood cells, so blocking all at once could harm normal blood cells,” said Dr. Gritsman. “However, there is evidence to suggest that these individual PI3K proteins can substitute for one another in normal blood stem cells, but not in some leukemic cells. So maybe we could stop AML by targeting one protein particularly crucial for survival of leukemic cells.”
But which one? By studying mouse knockout models, each lacking the gene for a different class I PI3K protein, Dr. Gritsman found that one—p110-alpha—is vital for leukemic stem cell survival and much less important for normal blood stem cells.
Next, she determined that those leukemias driven by mutations in the RAS gene seemed most dependent on p110α. “To test this hypothesis, we crossed a mouse model of RAS-induced leukemia with p110α knockout mice, which mimics the effect of using a p110α inhibitor to treat AML. And this led to a doubling in survival,” she said.
A Two-Pronged Therapy
That wasn’t the end of the story, since the mice eventually succumbed to leukemia. Dr. Gritsman surmised that it might be possible to strengthen p110α inhibition by simultaneously inhibiting another common cancer pathway—the MEK pathway. And in fact, this inhibitor combination proved to be a potent one-two punch in both tissue culture and mouse models of AML.
The results were so compelling that Dr. Gritsman was able to persuade the pharmaceutical company Novartis to expand an ongoing trial combining treatment with p110α and MEK inhibitors to include patients with RAS-mutated AML or myelodysplastic syndrome, another blood stem cell disease that frequently progresses to AML. Montefiore, Einstein’s University Hospital and academic medical center, has just joined this multicenter trial. Dr. Gritsman was recently awarded a 5-year, $2 million grant from the National Cancer Institute to support this research.
To learn more about the Albert Einstein Cancer Center, please visit www.einstein.yu.edu/cancer.
Posted on: Wednesday, June 22, 2016

Q: What is the status of kinase inhibitor therapy?
A: Quite a few kinase inhibitors are already approved for treating a range of cancers. These drugs interrupt the activity of kinases at different points in the signaling pathway. One of the best-known kinase inhibitors is imatinib (Gleevec), approved for treatment of chronic myeloid leukemia and gastrointestinal stromal tumors. Other kinase inhibitors include erlotinib (Tarceva) for lung cancer, and lapatanib (Tykerb) for HER2+ breast cancer. One of the most noteworthy kinase inhibitors is vemurafenib (Zelboraf), for treatment of late-stage melanoma. Responses are dramatic but can be short-lived.


Tablet Blog