

The Uganda Advantage
The Uganda Advantage: The Domestic Gain from Global Health Training
The beautiful Kisoro, Uganda countryside is marked by steep hills, towering volcanoes, and serpentine lakes only accessible by walking hours along dirt roads. For the villagers of this underserved region of Africa, a steady infusion of young, energetic American physicians has helped to improve access to quality medical care. These physicians return to the United States with stronger examination skills, improved bedside teaching and a more evidence-based, cost-effective work style.

Gerald Paccione, M.D.For eleven months of each year, Einstein faculty, residents and medical students join with Doctors for Global Health and Montefiore Medical Center, the University Hospital for Einstein, to staff Kisoro District Hospital (KDH), located in a largely rural area of southwestern Uganda, north of Rwanda and east of the Congo. When Dr. Gerald Paccione, professor of clinical medicine at Einstein and director of global education for the primary care and social internal medicine residency program at Montefiore, first visited Kisoro in 2005, he found that the needs of the villagers were stark –families typically had an average of eight children per household while subsisting on less than two dollars a day. Yet community members were warm, welcoming and eager to facilitate a sustainable partnership.
Kisoro has one doctor for every 40,000 people. Basic necessities such as sheets and mattresses are precious at this hospital, and there are few diagnostic tools beyond a centrifuge and microscope, as well as ultrasound and X-ray equipment that often are out of service.
Reclaiming the "Lost Art"
Rather than lamenting what KDH lacked, Dr. Paccione saw what it could offer: extensive opportunity for faculty and residents to learn how to conduct thorough physical exams and use critical thinking in place of tests. "To successfully treat patients in a place without resources, you have to be the instrument of the diagnosis," he explained. "Working in Uganda teaches us to practice effective medicine outside the hospital setting."

Transporting a patient into the hospital"When there's no chest X-ray or CT scan to double check your exam, you listen longer, percuss with better technique, and palpate deeper," said Dr. Samuel Cohen, a resident who was in Uganda in autumn 2012. "You think harder, because with less information there are fewer pieces of the puzzle."
Residents and senior medical students prepare for the Uganda experience through the prerequisite global health elective, which packs 150 hours of teaching time into four weeks and provides an intense introduction to global health from both public health and clinical perspectives. The course, and Uganda experience, recently received New York State accreditation for 12-credit Advanced Certificates in Global Medicine.
Each year, approximately 20 residents and 16 medical students travel to Kisoro to serve one-month rotations on the KDH medical wards and run the twice-weekly Chronic Care Clinic. Supervision is provided by a faculty member from the Global Health and Clinical Skills Faculty Development Fellowship (GHACS). Faculty members demonstrate cost-effective clinical skills refined through their own KDH experience. Near-daily e-mail exchanges with Dr. Paccione provide extensive discussion and coaching to augment the diagnoses of diseases, which can include advanced-stage malaria, tuberculosis, HIV, pneumonia, valvular and restrictive heart disease, diarrhea, and typhoid. Residents who are rounding in the Bronx also gain from the Uganda experience, through discussion of case studies concerning patients seen at KDH, and by gathering relevant literature for their peers in Uganda.
"This long-distance exchange facilitates learning on both sides," said Dr. Paccione. "While many residency programs bemoan the fact that their residents are only learning medicine by computer, our residents are perfecting their skills in the physical exam." "In my clinical work, I am continually developing my clinical reasoning and physical diagnosis skills in order to make management decisions that minimize unnecessary testing," noted Dr. Sheira Schlair, who helped establish the global health training program in 2007. "This is truly a life's work, and for me, these lessons were first learned in Kisoro."
The Payback
According to the Centers for Medicare and Medicaid Services, our nation's annual healthcare spending now surpasses $2.6 trillion. Physicians who receive global health training, however, may be able to help better control healthcare costs.
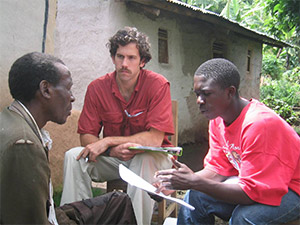
Interviewing a patientWithout a CT scan machine at KDH or at the Chronic Care Clinic, residents routinely practice the ability to hear a heart murmur, feel a spleen, hold an ophthalmoscope, or describe a rash or a node. " Our residents gain the skills necessary to make confident diagnoses, restrain the excessive use of tests, and operate comfortably and productively in a medical office," said Dr. Paccione.
"By the end of the month, I could quickly diagnose heart failure and its likely cause," said Dr. Christopher Knudson, a third-year resident. "I've told every intern considering cardiology that they must go to Kisoro."
"The emphasis on history and physical examination and the ability to refine those skills with Jerry was absolutely the most defining aspect of the experience," added Dr. Rohit Das, now chief resident of the Internal Medicine Training Program. "Such skills are overlooked in Western medicine, where easily available imaging studies have, to a certain extent, compromised the necessity to learn them."
A hospital without reliable diagnostic equipment, however, is hardly a utopia when it comes to patients'needs. "There are certainly times when I wish I had access to modern medicine," said Dr. Erin Goss, a faculty fellow. "An 18-month-old child came in with difficulty breathing, and needed oxygen and nebulized epinephrine, but the power was out. I had to transfer her to another hospital that had power. It's painful to not be able to give life-saving therapies to someone so young."
Those Who Teach
Internal medicine physician-educators with strong clinical skills may provide a solution to the rising need for healthcare cost containment. However, finding the right people for these roles requires the creation of attractive, career-building job options targeted to physicians willing to work for less in the interest of their ideals.

Education sessionA particularly innovative aspect of the Uganda program is its two-year GHACS fellowship, established in July 2012, through which four junior faculty members spend three months of each year in Kisoro and eight months at Montefiore. In Kisoro, faculty-fellows supervise residents, see patients and sponsor research projects in medical education, in clinical assessment and diagnosis and in community medicine. (Previous research has resulted in extensive programming to address issues such as malnutrition, literacy, and maternal mortality.)
At Montefiore, the faculty fellows cover evenings and weekends at the Comprehensive Health Care Center, supervise residents in researching and discussing patient cases sent from Kisoro, teach clinical reasoning and physical diagnosis and complete their Kisoro-based research projects. They emerge from their experience with strong hands-on skills, positioning them as outstanding medical educators.
"Our faculty fellows gain mentored experience in medical education, clinical skills and global health; Montefiore meets its ACGME requirements for supervision abroad and gets low-cost, enthusiastic medical educators who are experts in clinical skills and reasoning; and the Kisoro medical system benefits from dedicated, experienced clinical supervisors," said Dr. Paccione. "It's a true win-win-win."
A New Attitude
On many levels, physicians' time in Uganda is transformative.
"The Uganda experience rejuvenated me and reminded me of why I'd initially decided to become a physician," said Dr. Cohen. "I've returned home with a renewed interest in how we as physicians decide which tests to order."
"Working in Kisoro gave me so much more confidence," added Dr. Knudson. "I trust my own abilities, and I order far less testing and think more."
"I returned home with an inner confidence and clarity about my mission and skills as a future primary care physician that I can still appreciate now, five years later," agreed Dr. Schlair.
Posted on: Thursday, March 28, 2013

Tablet Blog