

FULL STORY
Q & A with Dr. Margaret Kielian
After evaluating evidence gathered from many studies over several months, the U.S. Centers for Disease Control and Prevention announced on Wednesday that the Zika virus, a member of the flavivirus genus, definitely causes microcephaly (unusually small heads and damaged brains) in infants born to infected mothers. Brazil has been especially affected by microcephaly cases caused by the virus. Zika virus also poses a significant public health threat to residents of other South America countries and to Puerto Rico and is predicted to reach the southern continental United States this summer. Little is understood about Zika virus, so we asked Margaret Kielian, Ph.D., a leading flavivirus researcher, to provide insight into how the virus genus behaves, explain what is known about the widening Zika problem, and describe the search for an effective vaccine. Dr. Kielian is a professor in the cell biology department and is the Samuel H. Golding Chair in Microbiology.
Margaret Kielian, Ph.D.Q: Your research focuses on how alphaviruses and flaviviruses enter and exit the cell. Is there anything unique or notable about flaviviruses compared with other viruses?
A: Before the recent publicity over Zika virus, the best-known flavivirus was dengue, responsible for more mosquito-borne infections than any other virus. Each year more than two million people develop dengue hemorrhagic fever, resulting in about 25,000 deaths. Zika and dengue not only belong to the same virus genus but also have the same mosquito vector, Aedes aegypti, which carries and transmits the virus. Aedes aegypti is also the mosquito responsible for transmitting another flavivirus—the yellow fever virus—which is present in tropical and subtropical areas of South America and Africa and can cause illness in non-vaccinated U.S. travelers to those areas.
One interesting aspect of dengue virus is that people with levels of anti-dengue antibodies insufficient to neutralize the virus can actually experience enhanced infection and disease after exposure to the virus. This is a major reason that developing a dengue virus vaccine has proven so challenging.
Q: Are there any other flaviviruses besides Zika virus that are known or suspected of passing from mother to baby through the placenta and causing congenital abnormalities?
 A: To my knowledge, Zika is the only flavivirus that can be transmitted this way. But rubella virus, a togavirus that is similar in several ways to Zika, causes the well-known congenital rubella syndrome (CRS) in babies when a pregnant woman contracts rubella, particularly during the first trimester of pregnancy. A very effective rubella vaccine has been available since 1969 that has basically wiped out rubella in North and South America—a real vaccine success story. But in those countries without strong vaccination programs, which account for approximately 60 percent of the world’s births, CRS is still a big problem, and approximately 100,000 babies with CRS are born per year.
A: To my knowledge, Zika is the only flavivirus that can be transmitted this way. But rubella virus, a togavirus that is similar in several ways to Zika, causes the well-known congenital rubella syndrome (CRS) in babies when a pregnant woman contracts rubella, particularly during the first trimester of pregnancy. A very effective rubella vaccine has been available since 1969 that has basically wiped out rubella in North and South America—a real vaccine success story. But in those countries without strong vaccination programs, which account for approximately 60 percent of the world’s births, CRS is still a big problem, and approximately 100,000 babies with CRS are born per year.
Q: Have any other flaviviruses besides Zika virus been shown to be neurotoxic?
A: Yes—West Nile virus is a good example, as it can cause encephalitis.
Q: How would you assess the health threat that the Zika virus poses to the U.S.?
A: From what I’ve read, the threat does not seem high right now, particularly given the mosquito control and exposure rates in the United States. But climate change, global travel and international commerce spread mosquitoes as well as pathogens. There have already been some 700 travel-associated cases in the U.S. including 69 pregnant women, and the data now indicate that the virus can also be sexually transmitted. So it’s important to keep on top of this and not assume that such mosquito-borne illnesses won’t happen here. Also, if the virus starts to be readily transmitted by the mosquito species Aedes albopictus (the Asian tiger mosquito), that would be an added concern, since its range extends further into the U.S. than Aedes aegypti.
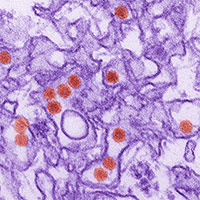
Zika Virus
Photo credit: Cynthia GoldsmithQ: An effective vaccine against one member of the flaviviruses—the yellow fever virus—was introduced in 1937. But it has proven difficult to develop vaccines or treatments for others. How optimistic should we be that a vaccine against the Zika virus can be developed soon?
A: There is a lot of basic information we still don’t know about Zika, including how difficult it would be to make a vaccine. But results reported recently in Science Translational Medicine for an experimental dengue vaccine could bode well for a Zika vaccine—especially since the dengue is so similar to Zika and has resisted efforts to develop an effective vaccine for nearly a century.
Q: What were the findings?
A: The dengue vaccine trial was a federally funded randomized double-blind “challenge trial” involving 41 healthy volunteers, with 21 of them receiving a single dose of the vaccine and the other 20 receiving a placebo vaccine. Six months later, all 41 were infected with a mild form of dengue. All 20 people in the placebo group developed rashes and other symptoms of dengue, while all 21 volunteers receiving the experimental vaccine remained healthy and had no evidence of infection in their blood. The same scientists who worked on this dengue vaccine have already developed vaccine candidates for Zika that may be tested in small human trials this summer. So I’m cautiously optimistic that an effective Zika vaccine may be possible in the not-too-distant future.
Posted on: Wednesday, April 13, 2016

Tablet Blog