

Sarnoff Fellowship Awardee
Sarnoff Winner Sarah Marx: Living in Two Worlds
Take a third-year Einstein medical student away from the hospital, place her in a laboratory equipped with microscopes and mice, and what happens? That’s what Sarah Marx, Class of 2019, is finding out. Sarah is one of just 10 recipients of a 2017–18 Sarnoff Medical Student Research Fellowship Award—a prize that supports students for a year in biomedical facilities other than their home medical schools.

Sarah with her Sarnoff Fellowship mentor, Dr. Paul Cohen (Photo Credit: The Rockefeller University)Since June, Sarah has been at New York’s Rockefeller University, in the laboratory of molecular metabolism, headed by Paul Cohen, M.D., Ph.D., the Albert Resnick, M.D., assistant professor at Rockefeller. “It’s a completely different type of thinking,” said Sarah. “You’ve been a medical student with a rule book telling you what to do, and suddenly, the rule book is thrown out and the whole point is to discover the new rules.”
Sarah applied for the award at the suggestion of Einstein’s Richard Kitsis, M.D., a professor of medicine (cardiology), and is the first Einstein student in 15 years to receive the fellowship. The Sarnoff Cardiovascular Research Foundation noted her undergraduate biomedical engineering degree from Yale and her interest in cardiology.
“In Uganda two years ago, I saw many children with heart failure from uncorrected heart problems,” she said. One nine-year-old girl’s story was tragic. “We sent her echocardiogram to pediatric cardiologist Daphne Hsu, M.D., and a radiologist at Einstein/Montefiore. The bottom line was that the girl needed surgery, but there wasn’t a single cardiac surgeon in Uganda.”
Sarah arranged for surgery in Kenya. The girl and her father made the 20-hour bus trip, “but the night before surgery, she passed away,” said Sarah. “It really brought home to me that where you’re born can determine health outcomes.”
Fats of Many Colors
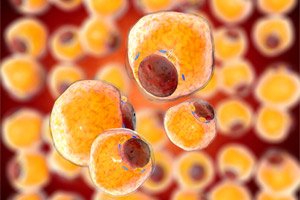
Fat cells from adipose tissue feature in Sarah’s study; she aims to understand how obesity induces hypertension and to develop targets for lowering blood pressureSarah is broadening her cardiology horizons in Dr. Cohen’s laboratory, whose guiding research question is “Can we break the link between obesity and disease?” Obesity contributes to metabolic disorders such as diabetes, hypertension and cardiovascular disease, and is also a risk factor for many types of cancer, but where excess adipose tissue (fat) is stored in the body strongly predicts whether these disorders will develop.
Obese individuals with the classic apple shape—adipose tissue around the middle, called visceral fat—often have low-grade chronic inflammation and metabolic disorders. Their fat contains white adipocytes (fat cells), which store energy in inert fat droplets.
Pear-shaped obesity tends to be associated with a lower burden of metabolic disease. While no studies to date have shown that subcutaneous tissue in humans stores beige fat, its presence is well proven in rodents; therefore, similar to the beige fat cells found in rodents, individuals with a pear “body type” may be mediated by the presence of “healthier” fat cells.
Brown adipocytes, a third type, behave like beige cells, are plentiful in infants and remain in adults around the upper chest and neck. Scientists are seeking the molecular controls that direct different types of fat to form, hoping to engineer healthier fat.
“In my project, we implanted blood-pressure devices in mice with different types of adipocytes,” explained Sarah. “We aim to understand how obesity induces hypertension and to develop targets for lowering blood pressure.”
She also studies the benefits of bariatric (weight-loss) surgery. “Mice that have stomach-reduction surgery consume more oxygen and can maintain weight loss because they use more energy and burn more calories. We think that surgery’s effects on fat play a role and hope to learn whether the fat remaining after weight-loss surgery is beige, white or brown.”
A Balanced Future
Dr. Cohen was delighted to welcome Sarah—his first Sarnoff student—to his lab. “Many of my most successful colleagues got their start as Sarnoff fellows,” he said. “Sarah is incredibly bright and motivated, and she has great insights into problems that combine her knowledge of medicine with her ability to think deeply about a scientific problem.”
As a physician-scientist who lives “both in the world of medicine and in the world of science,” Dr. Cohen models this integration himself.
“I’ve accompanied him to Memorial Sloan Kettering Cancer Center, where he’s an attending physician in the cardiology clinic,” said Sarah. “It has allowed me to see how a brilliant researcher and scientific thinker can also be a compassionate clinician.”
She added, “With Dr. Cohen’s mentoring, I’m getting a firm foundation in research so it can be a part of my life as a clinician.”
Editors’ Note: The Sarnoff Cardiovascular Research Foundation has helped medical students become leaders in cardiovascular innovation, research and medicine since 1979. It is named for Dr. Stanley Sarnoff, who invented technology to prevent heart attacks in soldiers exposed to nerve gas. Dr. Sarnoff died in 1990 while waiting for a heart transplant.
Posted on: Tuesday, May 22, 2018

Tablet Blog